Screening for high fracture risk
We're driving the research needed to establish the world’s first screening programme for high fracture risk, to ensure - No More Broken Bones. No More Broken Lives.
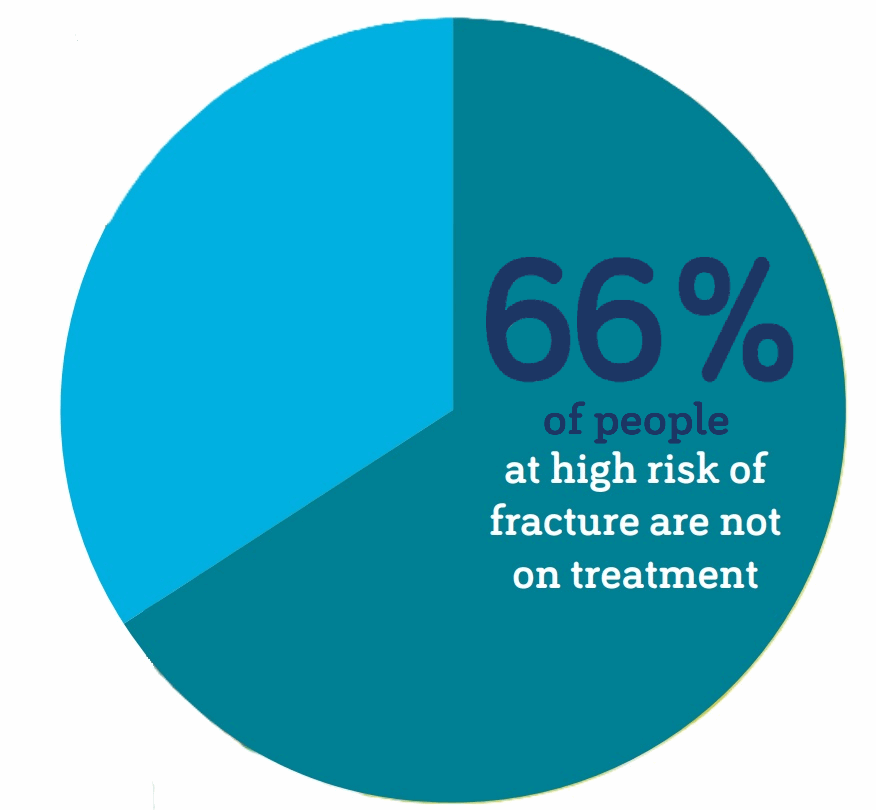
Osteoporosis is one of the most urgent public health crises of the modern era. Broken bones (fractures) caused by the condition are one of the most serious threats to living well in later life. Broken hips are heart-attack level events, as more than a quarter of people who break a hip, die within a year1. Late diagnosis and low public awareness mean at least two-thirds of people with osteoporosis are missing out on life-changing drugs2 .And in the case of broken hips, they are life-saving drugs. This costs the NHS a staggering £4.6 billion a year3, which due to our ageing population will be increased further. As it is predicted there will be a 25-30% rise in fractures by 20344.
What do we mean by screening for high fracture risk?
A screening programme aims to identify a condition when it's at an early stage where treatment can be effective to alter its course.
The UK National Screening Committee (NSC) defines targeted screening for high-risk groups, as: A nationally delivered proactive screening programme which aims to improve health outcomes in people with the condition being screened for, among groups of people identified as being at elevated/above average risk of a specific condition. Compared to the general population, the people targeted may have higher risk because of lifestyle factors, genetic variants or having another health condition. Targeted screening differs from population screening as it aims to identify groups of people with a higher risk of a specific condition beyond demographics such as age or sex. For example, individuals who smoke are at a higher risk of developing lung cancer regardless of their age or sex.
Targeted screening for high fracture risk: It is likely to include preselection of participants based on a fracture risk assessment tool (FRAX)* calculation or presence of clinical risk factors, followed by a bone mineral density (BMD)** measurement. BMD measurement alone has a low sensitivity for fracture risk and therefore its use for mass screening is limited. Easily accessible tools, such as the FRAX, estimate the individual ten-year probability of osteoporotic fractures based on clinical risk factors. Combining FRAX with BMD measurement has been proven to more effectively identify high-risk individuals for targeted treatment before they have a fracture.
* Fracture risk assessment tool (FRAX)– a computer tool that calculates your chance of breaking a bone (your ‘fracture risk’) in the next 10 years. There are a number of different tools available, such as FRAX® and QFracture®, which have been developed from results from different research trials. The tools include details such as your height and weight, and other risk factors linked to bone strength with some taking into account the results of your bone density scan. Find out more.
** Bone mineral density (BMD) - how much calcium and other minerals (called ‘bone mineral’) is in an area of bone, as measured by a DXA scan. This helps us to understand how dense and strong our bones are likely to be. Find out more.
Who would a screening programme for high fracture risk help?
In the UK, unfortunately the current clinical guidance (CG146) from the National Institute for Health and Care Excellence (NICE) isn't mandated. The guidance states the following people should be assessed for their risk of fragility fractures:
- all women aged 65 years and over
- all men aged 75 years and over
- women aged under 65 years with risk factors
- men aged under 75 years with risk factors.
In 2022, the All Party Parliamentary Group (APPG) for Osteoporosis and Bone Health, which the ROS convenes, released the results of its Inquiry into under-diagnosis of osteoporosis. The report revealed that 61% of people with one of the three major risk factors requiring a bone health assessment had not received one.
The inquiry showed that decisions are made by individual clinicians on a case-by-case basis. This is leaving thousands without the care they need and resulting in failure to prevent life-changing pain and disability. This is because, unlike other health conditions, there is no formal systematic national approach (i.e. screening programme) to identifying people at risk of osteoporosis and fractures.

“My name is Andrea and I’m 62. Five years ago, I was being treated for cancer. I found, though, that whenever I lay flat on the radiotherapy bed, or went for an MRI or CT scan, it was excruciatingly painful. I had great difficulty moving. So the hospital sent me for an x-ray on my spine. To my complete shock, it showed up several fractures. I then had a DXA scan that confirmed the diagnosis: I had osteoporosis. I was immediately prescribed alendronic acid together with calcium and vitamin D supplements that I still take today. When I think back now, it’s clear to me that the signs were already there. I had a history of back pain, and I’d been to see my GP about it on several occasions. But at no point did this pain, and the fact that I was a post-menopausal woman, trigger any suspicion that I might have osteoporosis. Sadly, at that stage I wasn’t referred for further investigations. Indeed, I was once told that a woman of my age should expect some aches and pains! Deep down, I knew that there was something wrong with my spine, but time marched on without having any treatment. In my opinion, had I been diagnosed years earlier, I would not have the spinal fractures and debilitating chronic pain that I have today.”
How could a screening programme for high fracture risk help?
The Inquiry into under-diagnosis of osteoporosis analysed the current evidence. It showed that a targeted screening programme to identify high fracture risk could be both clinically effective and cost-effective, especially in reducing hip fractures.
Why is there currently no screening programme for high fracture risk?
The UK National Screening Committee (UK NSC) has been making evidence-based recommendations on screening programmes for the past 28 years. The UK NSC is responsible for advising ministers and the NHS in the 4 UK countries about all aspects of screening and supporting implementation of screening programmes. Potential screening programmes that are within the UK NSC’s remit are considered on a case-by-case basis. The committee sets a high bar in assessing evidence against criteria which cover the condition, the proposed test(s), intervention, screening programme and implementation.
In 2019, a UK NSC review concluded to not recommend (population) screening for osteoporosis in postmenopausal women. The UK NSC recognised there was some evidence that hip fractures may be reduced by screening. But more research was needed to understand if this is correct. They stated that the direction of future research and reviews may benefit from focusing on a specific target sub-group (e.g. specific osteoporotic fracture).
This was followed in 2022, by the UK NSC’s functions expanding so it can now also actively consider targeted screening for high-risk groups. The recommendation for a targeted screening programme for high fracture risk is in line with Government’s own focus on prevention in the NHS Long Term. It is also consistent with the Chief Medical Officer, Professor Chris Whitty, commented in his 2023 Health in an Ageing Society report that a screening programme aiming for “a reduction in hip fractures may warrant further investigation”. Professor Whitty went on to say “This highlights an area of ongoing research which will inform future reviews regarding national screening programmes for targeted populations” .
To establish a targeted screening programme for high fracture risk, all the UK NSC criteria for appraising the viability, effectiveness and appropriateness of a targeted screening programme have to be met. To demonstrate this, the robust evidence must be available.
What further evidence is needed to support the case?
Previous published studies propose that the further research required to support the case for screening for high fracture risk should focus on implementation of a programme. For example:
- How should a screening programme for high fracture risk be approached in real-life settings? Need to address the lack of data and garner the robust evidence for the most efficient and acceptable systematic screening approach e.g. to enhance screening uptake, use of digital detection tools 5,6.
- How should a screening programme for high fracture risk be facilitated and maintained? Need to ensure systematic screening in routine care can be optimally effective and practical, considering access to bone density scans, information provision to participants and mode of administration7,8.
- What strategies will enable increased participation and intervention success? To optimise the effectiveness of the systematic screening, need to evidence approaches within the programme which will ensure improved participation and adherence to medication5.
We recognise that the current evidence base has focused on older women (aged over 65 or 70) due mainly to practicality and the need for efficient use of research funding. Incidence of fractures is higher in older women, so fewer study participants are required. However, we know that there is a care gap in osteoporosis for men, with costs of hip fracture shown to be higher for men. Therefore in line with the Equity strand of the ROS strategy, we support that any screening programme should not be limited to a population of older women (aged 70 and over), or the outcome of hip fracture alone.
For further information, please see the list of screening for high fracture risk related publications.
How does this ambition relate to ROS’s overall strategy?
We endeavour to put the patient voice at the heart of everything we do. We also know that identification of the condition early, continues to be one of the top priorities from a patient perspective.
Our new mission is to achieve a future we all want: No More Broken Bones. No More Broken Lives.
By 2030, we want to make sure that no-one has to live with the pain of untreated osteoporosis, through ground-breaking research - We’re driving world-class medical research that will give everyone earlier diagnosis and better treatment – starting with the world’s first screening programme.
This objective aligns with the ROS Breaking the Silence Strategy as we want to:
- Identify people who are at risk of breaking bones and make sure treatment is offered to prevent the first fracture. An early warning can help get people into the system, tackling under-diagnosis and sparing them the pain of avoidable fractures (Prevention).
- Concentrate on influencing the care of people who are at high risk of fracture who need to be targeted (Influencing Care).
- Generate and apply evidence to real-life settings, making sure breakthroughs are quickly put into practice, so that advances in research rapidly make a difference (Influencing Care).
- Focus our grants on studies that have a clear and tangible path to benefiting patients and which help drive system change (Influencing Care).
This objective aligns with the ROS Research Roadmap as we want to:
- Optimise the effectiveness of assessment and treatment. For example, the development of an integrated approach to ensure universal access to automated fracture risk assessment in primary care, was a key priority identified.
- Improve the bone health lifecourse by minimising fracture risk, to ensure fracture free health ageing.
How you can help
Latest news and updates
- Keele University to lead new £4.8million NIHR study to improve early diagnosis of osteoporosis
- New research funding awarded to build the case for world-first screening programme for fracture prevention
- New research funding announced to drive screening for high fracture risk
- "War on osteoporosis" campaign, run by the Mail on Sunday
 Search
Search
 Login
Login