
Osteoporosis Resources for Primary Care: Introduction
Introduction to osteoporosis
Osteoporosis is 'a skeletal disorder characterised by compromised bone strength predisposing a person to an increased risk of fracture' (NIH Consensus Statement 2000).
Fractures that occur because of reduced bone strength are described as ‘fragility fractures’ and many of these will be caused by osteoporosis.
NICE describes osteoporosis as 'a progressive skeletal disorder [...] characterised by low bone mass and deterioration of the structure of bone tissue leading to an increase in bone fragility and risk of fracture'. Patient experts involved in the production of the NICE Technology Appraisal of bisphosphonates explained that "fractures can be painful, have a significant impact on a person’s independence and increase mortality" and the "clinical experts emphasised that it is important to prevent fragility fractures, particularly in people at the highest risk of fracture". NICE concluded that "osteoporotic fragility fractures are debilitating, also affecting family and friends, and that preventing these would preserve the quality of life of the person and their carers."
Healthy bone:
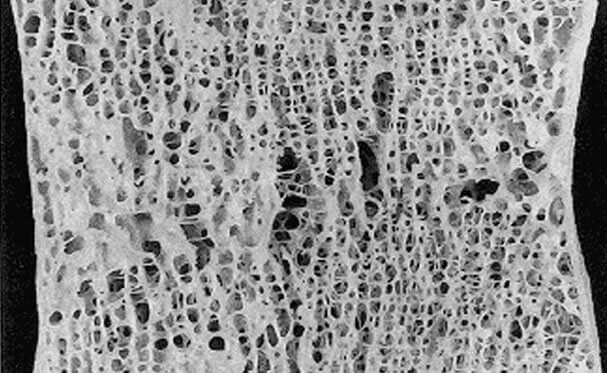
Osteoporotic bone:

Osteoporosis can be diagnosed via a bone density scan (although this is not always required). A bone density scan, using a densitometry X-ray (DXA), measures how much ‘bone mineral’ is in the area being measured – usually, one hip and the lower part of the spine. Research has shown that the lower the patient's bone density is the greater their risk is of having a fracture. The scan results are commonly given as a ‘standard deviation’ (SD) – the number of units above or below average. If the patient's bone density is 2.5 SD below average, this is described as ‘osteoporosis’. If the patient's bone density is between the lower end of the normal range and the ‘osteoporosis’ range, they are said to have 'low bone mass' (sometimes termed 'osteopenia’).
What are the causes of osteoporosis?
Osteoporosis occurs when bone remodelling – the balanced process by which bone is renewed and repaired – is disrupted by a variety of factors, some of which can be modified and some of which cannot at present. It is thought that the potential for any individual to develop osteoporosis is determined by both genetic and environmental factors. These in turn determine:
- The peak bone mass achieved at maturity
- The age at which bone loss starts
- The rate of bone loss
A variety of risk factors increase the risk of fracture, and many of these do so by increasing the risk of osteoporosis. These risk factors will be covered in the Identification section of this resource.
What is the impact of osteoporosis?
Fragility fractures
Fractures that occur because of reduced bone strength are described as ‘fragility fractures’ and many of these will be caused by osteoporosis.
Fragility fractures consume vast health and social care resources. The number of incident fractures predicted in 2025, taking into account demographic projections, has been estimated at 682,000 in the UK. This represents an increase of 146,000 fractures from current levels. Hip, clinical vertebral (spine), forearm and other fractures have been predicted to increase by an estimated 23,000, 18,000, 15,900 and 89,300 (Svedbom 2013). Moreover, people with one or more long-term conditions, such as osteoporosis, account for around 70% of all hospital admissions and 70% of total NHS spending (Department of Health 2012).
“In the UK, an estimated 500,000 new fragility fractures arise each year, comprising approximately 79,000 hip fractures, 66,000 vertebral fractures, 69,000 forearm fractures and 322,000 other fractures” (Svedbom 2013).
Wrist fractures
A broken wrist can be the first indication that someone has osteoporosis. Wrist fractures in women often occur soon after the menopause and typically occur following a fall. Healthy bones should be able to withstand a simple fall so a broken bone in these circumstances, without any other disease, is an indication that there may be underlying osteoporosis.
Hip fractures
The National Hip Fracture Database annual report (2016) states that hip fractures take up £1.5 million worth of bed days (England, Wales and Northern Ireland only). It is estimated that the cost to hospital services of incident hip fracture is £1.13 billion (Impact of hip fracture on hospital care costs: a population-based study, by Leal et al).
"1 in 4 people (28.7%) die within a year of suffering a hip fracture” (Neuburger, et al 2015).
Vertebral fractures
There are currently 66,000 vertebral fractures each year and these are often undiagnosed. Vertebral fractures are the most common osteoporotic fracture. Studies suggest that 12% of older women have vertebral deformities, the majority of which will be osteoporotic in origin - increasing with age to 20% (women over 80 years of age). The impact of vertebral compression fractures is significant, causing chronic back pain, limitation of activity and impaired quality of life. 58% of people who have experienced spinal fractures are in long-term pain which they don't think will ever go away (NOS Life with Osteoporosis, the Untold Story).
“50 – 70% of vertebral fractures are undiagnosed." (NICE TA161 2008).
 Search
Search
 Login
Login

