
Vertebral fracture identification toolkit
Our vertebral fracture identification toolkit includes a set of clinical pathways and audit tools. These are designed to help you:
- establish pathways for vertebral fracture patients
- support quality improvement for vertebral fracture identification
- predict how many vertebral fractures you should expect to see in your area
- develop a business case to support better identification and management of vertebral fractures within fracture liaison services (FLS)
Clinical pathways
Use our clinical pathways to establish best practice care for vertebral fracture patients, from identification to secondary fracture prevention.
General fragility fracture pathways
These pathways can be used if you don't have access to a FLS in your area. They define best practice secondary fracture prevention for Scotland, England, Wales and Northern Ireland:
Vertebral fracture pathways
This pathway can be used to support appropriate management for patients with newly-identified vertebral fractures who are referred from imaging departments:
These pathways can be used to support secondary fracture prevention in different scenarios.
Within FLS:
These have been updated to include definitions of the role and competencies of HCPs reporting vertebral fractures within FLS services.
- New vertebral fracture (2022)
- Previously unreported vertebral fracture (2022)
- Previously unreported vertebral fracture identified during a DXA vertebral fracture assessment
In the absence of FLS:
Quality improvement
These pathways support decision making for the management of new vertebral fractures. They can be used to support quality improvement programmes in vertebral fracture identification:
Case Studies- integrating vertebral fracture identification into FLS
These case studies share methods for integrating vertebral facture identification into a Fracture Liaison Service and highlight some of the barriers experienced.
You can use the learning from these case studies to support your own service development.
Evolving strategies
Vertebral fracture identification strategies for FLS at Yeovil have been evolving:
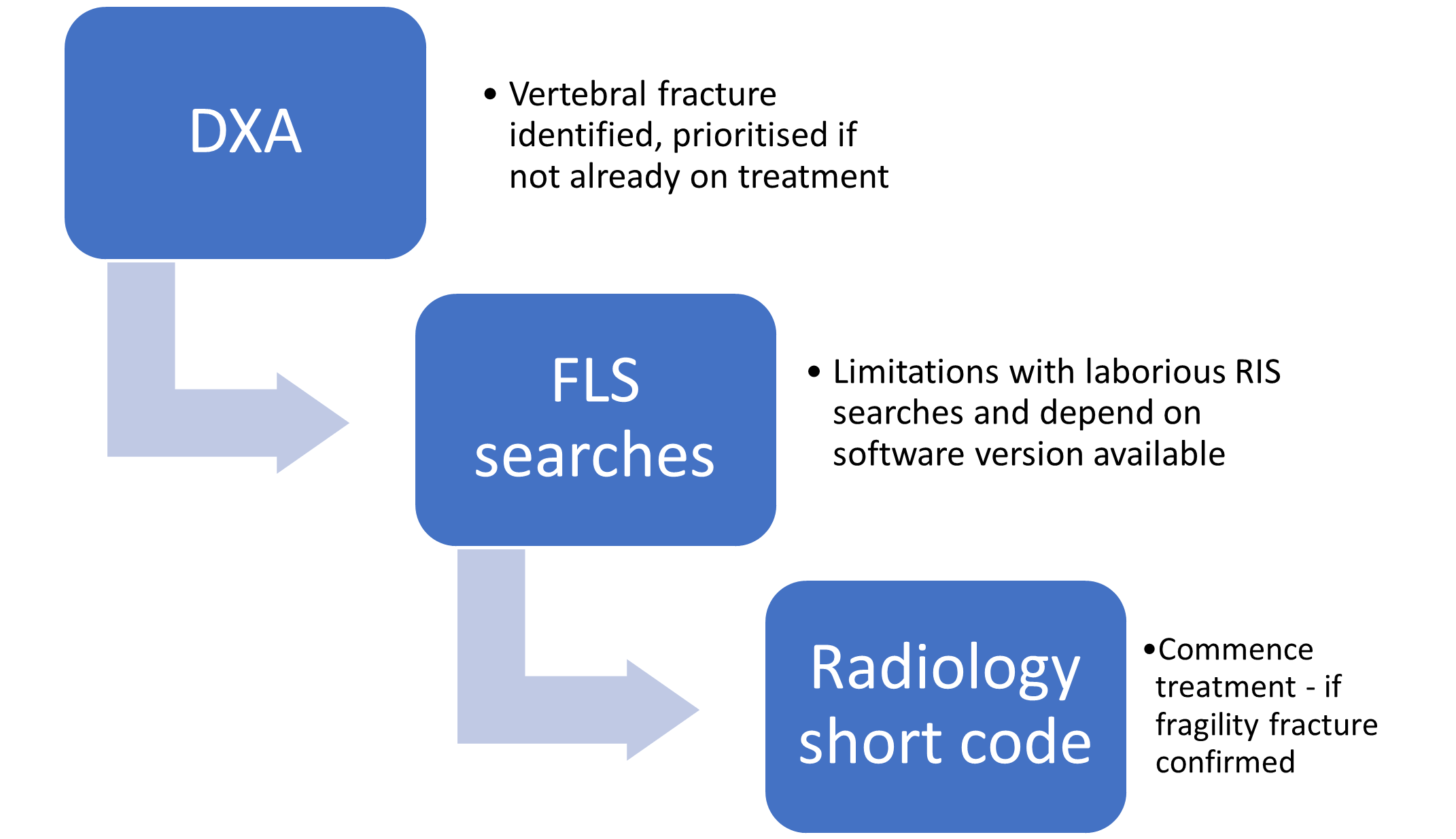
Many are identified through DXA referrals and there has also been a trial involving systematically reviewing imaging reports for vertebral fracture through radiology information system (RIS) searches.
There are limitations with identifying patients through FLS searches because not all are diagnosed in the Emergency Department and few are identified through discharge coding
In 2016 a systematic radiology search for vertebral fractures was trialed however this was limited by:
• the skill set of the administrator performing the searches (although she was a retired MIU nurse),
• the ability to search multiple phrases in radiology reports such as: crush, wedge, depression etc.
• the capacity of the clinical FLS team to manage the increased investigation to verify vertebral fractures and their acuity
The FLS nursing team also did not have the capacity to support these patients, manage their treatment plans and perform adequate follow ups.
Clare Cockill, FLS Nurse explains a new trial strategy:
’Since the RCR audit last January I agreed a phrase (after discussions about acceptability) with radiology that encourages GPs/referrers to consider starting treatment in patients with a newly identified vertebral fracture. This is currently a challenge to audit because we cannot search our current RIS version for the agreed phrase:
‘Appearances suggest osteoporosis. Exclude previous historical trauma as a cause of fracture and consider starting appropriate bone protection treatment.’
Correct reporting of vertebral deformities/fractures by the radiology team is an ongoing challenge. Since attending the Vertebral Fracture Identification course in Sheffield in 2018 I have had increased knowledge and confidence to be able to challenge radiology reports where fractures are being over- or under-reported. This expertise is essential where the treatment decision rests on whether or not a fracture is confirmed. I have also developed good links with the MSK radiologist who will review images where I need additional confirmation.’
Somerset Foundation Trust - Musgrove Park Hospital
Radiographer: Rosie James talks about their experience with embedding vertebral fracture identification into the FLS and the benefits of close links with Radiology.
Audit tools
Use our audit tools to understand how well your service is identifying vertebral fractures and find opportunities for quality improvement.
These can be used as part of routine clinical audit and quality improvement cycles, and can be adapted for your department's needs.
For CT scans
This tool helps to evaluate the identification of opportunistic vertebral fractures via CT scans.
This tool includes:
- audit criteria
- data collection sheet
- audit reporting template
- definitions of a vertebral fracture
To use this tool, you'll need to be confident in assessing sagittal spine CT images to identify vertebral fractures, and have access to original clinical radiology reports.
For referrals to DXA services
Audit tool for referrals to DXA
This tool can help you to learn:
- the proportion of referrals to your DXA service that indicate vertebral fractures
- the referral source
- whether there were previous missed opportunities to identify vertebral fractures
It includes:
- audit criteria
- data collection sheet
- audit reporting template
This tool could inform a business case for service development (for example, the introduction of vertebral fracture assessment to a DXA service), and help you understand how DXA could drive demand for FLS as a previously unexplored pathway.
For spine pathways
This tool is for evaluating the identification of vertebral fractures via spine pathways (for example, musculoskeletal or back pain services). It can help to establish whether these spine pathways may be a good place to identify vertebral fractures, and whether patients with vertebral fractures are being reported.
It includes:
- audit criteria
- data collection sheet
- audit reporting template
- definitions of a vertebral fracture
To use this tool, you'll need to be confident in assessing spinal imaging to identify vertebral fractures, and have access to original clinical radiology reports.
Business case tools
This is a tool for predicting the increase in demand on your FLS if you begin searching for incidental vertebral fractures on imaging.
This tool can help to:
- drive service improvement
- inform a business case for service development
- inform a business case for a new FLS, spinal service, or vertebral fracture FLS
It includes:
- instructions for use
- audit criteria
- data collection sheet
- reporting template for audit report and demand report
- definition of a vertebral fracture
- management pathway for secondary fracture prevention
To use this tool, you'll need to be confident in assessing sagittal spine CT images to identify vertebral fractures, and have access to original clinical radiology reports. You'll also need to know how many CT scans you complete in an average month or year.
Vertebral fracture identification benefits calculator
This tool is designed to estimate the benefits to patients and NHS costs in identifying vertebral fragility fractures, and treating the underlying causes.
The Calculator promotes effective case finding, assessment and treatment according to prevailing clinical guidelines and best practice at the time of use. The Calculator includes the option of selection of alternative pharmaceutical therapies for a cohort of patients
The Calculator has been designed for use by individuals who are able to support clinicians, business managers, commissioners and others
It includes:
- introduction and instructions
- inputs for local population, current and additional cases
- calcuation of the number of fractures expected for population, fractures prevented and the costs benefits for fracture prevention
For healthcare professionals
Our toolkit is supported* by:
*Amgen has provided financial support for this work but has not inputted or influenced its development.
 Search
Search
 Login
Login

 jill.griffin@theros.org.uk
jill.griffin@theros.org.uk
